Every one of us are prone to a fungal infection, even healthy people are no exceptions. Fungi are commonly found in the environment, and all of us breathe in or come in contact with fungal spores every day without getting ill.
[the_ad id=”13371″]
However, if you fall in the category of people with weak immune systems, these fungi are more likely to cause an infection. Infections that happen because a of person’s weak immune system are called opportunistic infections.
What weakens your immune system?
- Affected by uncontrolled diabetes (High blood sugar levels)

- Recovery from COVID-19
- Cancer & other comorbidities
- Continuous usage of steroids
- Using immune-suppressant medication
- Voriconazole therapy
- Poor hygiene (use of unfiltered water)
- Premature infants
- HIV/AIDS
- Transplantation, immunocompromised patients
What is Mucormycosis?
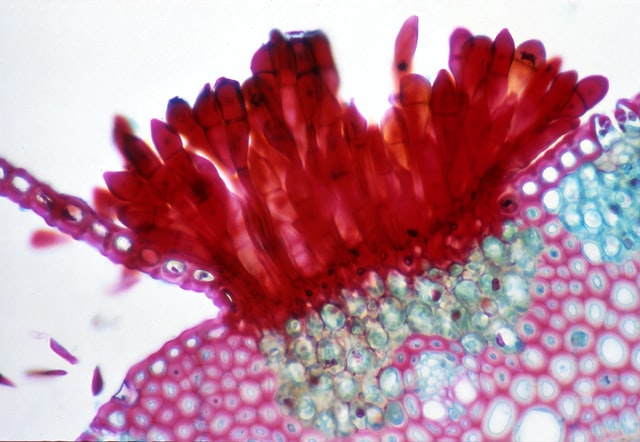
Mucormycosis also called Black/White Fungus or Zygomycosis is an invasive, fungal infection caused by a group of moulds called Mucormycetes which are present all over the environment, in soil and in association with decaying leaves, compost piles, and animal dung. They are more common in soil than in air, and in summer and autumn than in winter or spring. Most of us come in contact with tiny fungal spores every day, so it’s probably impossible to completely escape contact with Mucormycetes.
How does someone get Mucormycosis?
You may get Mucormycosis when you come in contact with fungal spores in the environment. For example, if you inhale the spores from the air, you may get infected with lung, sinus, orbit or brain forms of the infection.
The fungus may also cause a skin infection after it enters the skin through a scrape, burn, or other type of skin injury.
Gastrointestinal Mucormycosis is acquired by ingestion of fungus in foods such as fermented milk, dried bread products and fermented porridge .Alcoholic drinks derived from corn may promote gastric Mucormycosis .
5 Major clinical forms of Mucormycosis
According to Centre for Disease Control and Prevention (CDC), of the 5 major clinical forms of Mucormycosis; rhinocerebral and pulmonary infections are the most common.
- Rhinocerebral mucormycosis is an infection in the sinuses that can spread to the brain.
- Pulmonary (lung) mucormycosis symptoms are non-specific and include fever, cough, chest pain, and dyspnea
- Cutaneous mucormycosis may be primary or secondary. Primary infection is usually caused by direct inoculation of the fungus into disrupted skin and can occur in patients who are not immunosuppressed.
- Gastrointestinal mucormycosis is less common than the other clinical forms and is believed to result from ingestion of the organism. The most commonly affected are stomach, colon, and ileum.
- Disseminated mucormycosis may follow any of the forms of mucormycosis and the most common site of spread is the brain, but the spleen, heart, skin, and other organs can also be affected.
Symptoms and Warning signs of Mucormycosis
- Toothache, loosening of teeth, jaw involvement.
- Blockade of nasal passage or congestion (Sinusits) , discharge from nose (blackish/bloody),
- One-sided facial pain, local pain on the cheek bone, numbness or swelling
- Blackish discoloration over bridge of nose/palate
- Double or Blurred vision with pain; fever, skin lesion, thrombosis & necrosis (eschar)
- Chest pain, lung effusion, worsening of respiratory symptoms
- Periorbital swelling and pain
How is Mucormycosis diagnosed?
While diagnosing Mucormycosis/ Black fungus infection , a doctor consider your medical history, symptoms, physical examinations, and laboratory tests. If he suspects that you have Mucormycosis in your lungs or sinuses, then a sample of fluid might be collected from your respiratory system to send to a laboratory. Doctor may also suggest imaging tests such as a CT scan of your lungs, sinuses, or other parts of your body, depending on the location of the suspected infection.
What is the anti-fungal diet for Gastrointestinal Mucormycosis ?
- There are much more bacteria than fungi in your gut, and therefore, the good bacteria keep the fungi in check. However, taking antibiotics, immunosuppressants or having a disease that weakens your immune system can affect the balance of your gut bacteria.
- The fact is that your health will improve if you get rid of the extra fungi and re-introduce good bacteria into your gut. The basic idea is that the yeast feed on sugar and hence, sugar must be avoided.
- Diet low in sugar, yeast, refined carbohydrates, and mold-containing foods will create unfavourable conditions for fungal growth.
- Intake of Probiotics from yogurt, fermented foods, or supplements will enhance the good gut bacteria .
Can Mucormycosis be prevented?
- Maintain oral hygiene – Post recovery from Covid-19, the earlier intake of steroids or medications facilitate the bacteria or fungus in the mouth to grow and cause issues in the sinus, lungs and the brain. Maintaining oral hygiene by taking care of the mouth is a necessity which can be made certain by regular brushing and even taking oral clean ups.
- Avoid steroids– If you had taken high doses of steroids, then it may lead to high blood sugar levels and a high chance of Mucormycosis.
- Personal hygiene -One should ensure personal hygiene, wearing face masks and face shields to keep infections at bay.
How is Mucormycosis treated?
Mucormycosis is a serious infection that can be treated with antifungal medicine, usually Amphotericin B, Posaconazole, or iIavuconazole. These medicines are administered either through a vein (amphotericin B, posaconazole, isavuconazole) or by mouth (posaconazole, isavuconazole). Often, Mucormycosis may require surgery to cut away the infected tissue if not handled timely.
Source