Genetic testing can provide a personalized approach for clinicians to treat patients. It can help them prescribe an
[the_ad id=”6154″]even more individualized treatment plan, taking into account a patient’s own genetic makeup, in addition to the medical history, environmental and lifestyle factors that clinicians already consider when treating patients. Since every patient is unique, personalized medicine, including genetics, can help provide a treatment plan that is a better match.
Not all genes will express themselves. Some confer a propensity or a vulnerability to disease and can get switched on or off by our environment. This ‘environment’ comprises food, exercise, supplements, etc., and can be modified via strategies aimed at reducing these environmental triggers and, potentially, the overall risk for a particular disease. Recently, epigenetics has created a big buzz and refers to — over-simplistically, of course — the phenomenon of how our environment can modify the expression of our genes. Further, gene editing technologies like CRISPR hold the exciting potential to edit “faulty” genes and “cure” genetic diseases. A discussion about how far we can — or, should — go, is a topic for another post. But, overall, in genomics, it is fair to say we’re on the cusp of a near future when we will be able to take advantage of this cutting-edge technology that will one day be integrated in routine clinical care. But did you know there was a genomics-based test that has immediate application to daily clinical care? Allow me to introduce you to pharmacogenomics.
Pharmacogenomics combines pharmacology (the study of drugs) and genomics (the study of genes and their function) to provide invaluable information about how an individual’s DNA influences the response to medication. We know that a drug that works well in one person might not be effective for another or worse, may even cause unwanted side effects.
The problem with trial-and-error approach:
 This is because the way that a particular medication works depends on how it is broken down, utilized and eliminated by our bodies. For many drugs, this mechanism is determined by our DNA. And this is why pharmacogenomics represents personalized, precision medicine.
This is because the way that a particular medication works depends on how it is broken down, utilized and eliminated by our bodies. For many drugs, this mechanism is determined by our DNA. And this is why pharmacogenomics represents personalized, precision medicine.
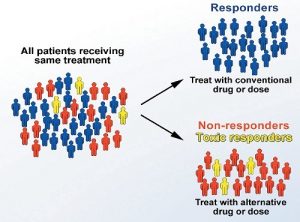
While we’re all over 99.9% similar to one another, the remainder 0.1% difference in our DNA can mean the difference between effective medication, a medication that doesn’t work, or one that produces a bad side-effect or an allergic reaction. Pharmacogenomics plays an important role in distinguishing between responders and non-responders to medication, identifying those at risk for a serious side effect, and also determining optimum drug dosage.
Pharmacogenomics tests are typically once-in-a-lifetime tests that are especially useful in choosing the right drugs for pain management, heart disease, cancer, diabetes, psychiatric conditions and antibiotics among others. In fact, the US FDA has listed over 200 drugs with pharmacogenomic markers for drug labelling that can provide information including:
● Variability in clinical response variability
● Risk for adverse events
● Dosing
● Mechanisms of drug action
This approach ushers in precision medicine that is personalized, informed, and aimed at:
● Maximizing drug-choice effectiveness
● Optimizing drug dosage, and
● Minimizing the risk of unwanted/harmful side effects
According to U.S Department of Health & Human Services, “over 770,000 people are injured or die each year in hospitals from adverse drug events”. Pharmacogenomics can play a vital role in reducing these numbers. Precision medicine can not only significantly reduce cost, disease exacerbation, adverse events and deaths associated with a trial-and-error approach, but also increase compliance and overall wellbeing. This is extremely useful to both prescribing physician as well as patients. In fact, physicians across the globe- as well as in India- have already started to use pharmacogenomic testing for its actionable results, and to narrow down treatment options. Understandably, for doctors as well as for patients, it can be extremely helpful just knowing that the drug they are prescribed is personalized and precise.
If you are curious about your response to medication, or if you feel that the medication you are on is not effective, all you have to do is to talk to your doctor, who can arrange for the test.
Source:

